

PRACTICAL HELP, TIPS & NEWS


WALLY BAK TALKS TO STUDENTS
14/03/2024

NDIS SUPPORTS LARONIX RESEARCH
05/10/2023

ENABLE NSW INCREASES ALLOWANCES
28/09/2023

FATHER’S DAY RAFFLE WINNERS
21/08/2023
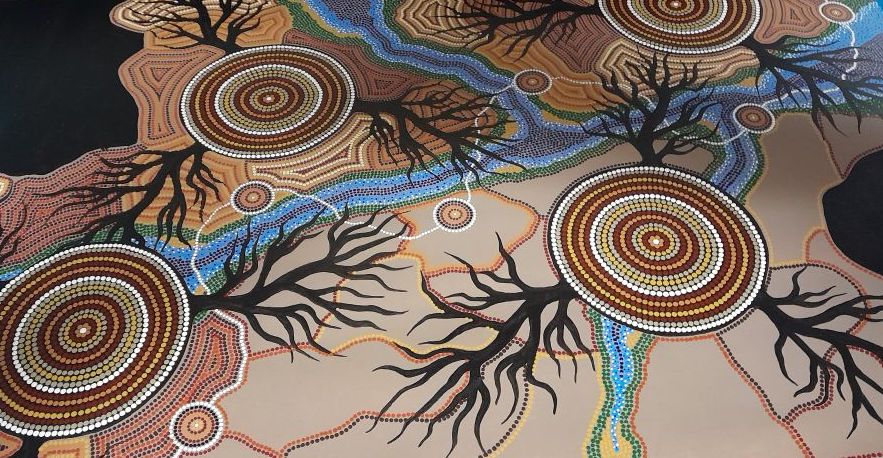
STEVE COATES STUNNING ART
18/07/2023

FATHER’S DAY RAFFLE TICKETS ON SALE NOW
29/05/2023

HEAD AND NECK CANCER AWARENESS
18/04/2023

TRAILERS 2000 GENEROUS DONATION
27/03/2023