
We provide support, assistance, comfort and friendship to everyone affected by laryngectomy surgery.
We understand how laryngectomy surgery can completely change your life.
You may feel anti-social, uncomfortable with talking in group situations or noisy environments, or feel lost and cast adrift from daily life.
Support from others in similar situations can help you navigate this journey.
Remember – your speech therapist is also your best friend!



“You can say that again” – introducing our eBook
Since 1989, we have provided a handy, printed guide to help laryngectomees adjust to their new way of life.
The eBook is your easy reference as you face the challenges of laryngectomy surgery with confidence and support. You’ll find a wealth of resources here, all based upon medical expertise and best practice and delivered in a warm and easy-to-read manner.
We don’t expect you to go it alone with just this eBook. Our website can help you find resources, provide helpful tips and connect you with support groups to help you on your journey.
Take a look at our ‘You Can Say That Again’ eBook, or get in touch with our Welfare Officer to discover more.
Welcome to the laryngectomee association of NSW
Our team can support you as you regain your love of life — your love of you!
We are on your side, helping you deal with the trauma of surgery, post-radiation, or chemotherapy, and creating a route to effective healing and management of symptoms.
Our Story
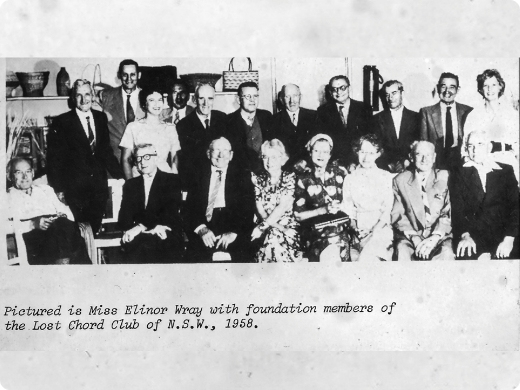
Our work builds on that of Elinor Wray, a speech therapist who founded the Lost Chord Group back in 1958.
While Elinor is sadly no longer with us, her commitment and her work live on in our support groups and services.
Regain control
Grow your confidence and regain your love of socialising. Meet other laryngectomees and learn more about the stories of people in a similar position to your own.
Whether you are a laryngectomee, a partner or a carer, you’ll find support and friendship in a safe, caring space.


Here to support you
We provide personal, friendly help to all laryngectomees and persons with similar communication difficulties.
Our dedicated welfare officer Yvonne Byrnes, the wife of our President and fellow laryngectomee Les Byrnes, oversees our support and welfare assistance.
